Vitrification and Fertility Preservation
Vitrification plays a crucial role in fertility preservation, offering hope to individuals who may face fertility challenges in the future. For women undergoing cancer treatment, vitrification allows for the preservation of oocytes before chemotherapy or radiation therapy, which can harm reproductive cells. This gives cancer patients the opportunity to have biological children after their treatment.
Vitrification is also beneficial for women who wish to delay childbearing for personal or medical reasons. By preserving their oocytes at a younger age, women can increase their chances of having a successful pregnancy later in life when their natural fertility may have declined. This option empowers women to take control of their reproductive future.
Vitrification is a current rapid cryopreservation technique that is routinely used to store Human Oocytes, Cleavage Stage Embryos, and Blastocysts for future use. This procedure supports cell survival by preventing ice crystal formation within cells. The formation of ice crystal is damaging to the cellular ultra-structure by physically breaking the plasma membrane and organelles. The vitrification process removes all of the water within the oocyte, embryos or blastocysts, transforming the cells cytosol into a glass-like state. This method is widely used in IVF laboratories worldwide and has produced high survival rates and minimal cellular damage, successfully preserving human oocytes, cleavage stage embryos, and blastocysts.
The Science Behind Vitrification
The term “vitrification” comes from the Latin word “vitreum,” meaning glass. In the context of cryopreservation, vitrification refers to the transformation of a liquid into a solid glass-like state without forming ice crystals. This process involves two critical steps: the use of cryoprotectants and ultra-rapid cooling.
Cryoprotectants are substances that protect biological tissue from freezing damage. There are two main types of cryoprotectants used in vitrification: permeating and non-permeating. Permeating cryoprotectants, such as imethyl sulfoxide (DMSO) and ethylene glycol, penetrate the cell membrane and replace water inside the cells. Non-permeating cryoprotectants, like sucrose and trehalose, stay outside the cells and help dehydrate them, reducing the amount of water available to form ice crystals.
Ultra-rapid cooling cools embryos to -196 C temperature at cooling rates exceeding 10,000 C/minute. This is critical to ensure that embryos spend minimum time in the required highest concentration of cryoprotectants, which can be toxic for embryos if their exposure is prolonged beyond a minute.
Vitrification in Clinical Practice
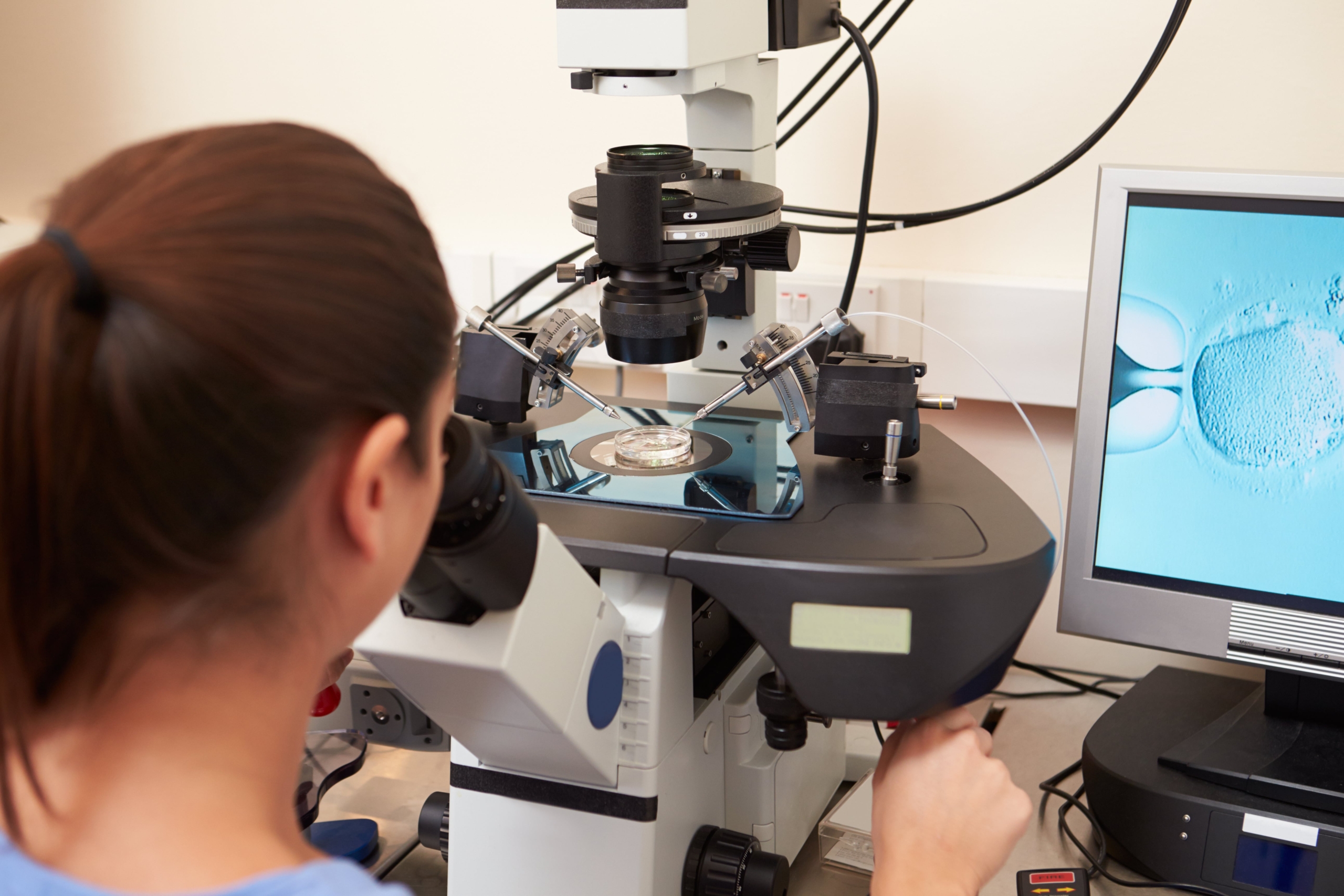
Vitrification is widely used in fertility clinics around the world. It is a standard practice for ‘freezing’ or cryopreserving oocytes and embryos in IVF treatments. The technique has also been successfully applied to preserve ovarian tissue, which can be used for fertility preservation in cancer patients.
The process of vitrification is highly standardised, with strict protocols in place to ensure the highest quality and safety of the preserved cells. Clinical embryologists undergo specialised training to master the technique and achieve consistent results. This standardisation has contributed to the widespread adoption and success of vitrification in ART.
The vitrification and warming of oocytes and cleavage stage embryos involves several critical steps:
- 1) Incubation in Equilibration solution: The oocytes or embryos are first exposed to an equilibration solution containing cryoprotectants, which helps to dehydrate the cells and introduce intracellular protective agents. The equilibration process allows cryoprotectants to replace water inside the cells, preventing ice formation when the cells get to ‘freezing’ temperatures. The cells are typically placed in a series of solutions with increasing concentrations of cryoprotectants to gradually dehydrate them.
- 2) Incubation in Vitrification Solution: Once the cells are partially dehydrated, oocytes or embryos are moved to a solution with even higher concentration of cryoprotectants and loaded into cryodevices, for example straws, in a minimum amount of solution.
- 3) Rapid Cooling: The cryodevices are then quickly plunged into liquid nitrogen, the resulting ultra-rapid cooling rate ensuring that the cells turn into a glass-like solid without forming ice crystals. The entire process happens in a matter of seconds.
- 4) Storage: The vitrified oocytes or embryos are then stored in liquid nitrogen at -196°C. At this temperature, all metabolic processes stop, and the cells can remain viable for years. Specialised storage tanks are used to maintain the ultra-low temperatures and ensure the long-term viability of the cells.
- 5) Warming: When the vitrified oocytes or embryos are needed for use, they are rapidly warmed to avoid the formation of ice crystals during warming. In this process cryodevice containing oocytes or embryos is removed from liquid nitrogen, opened and the section containing the oocyte or embryo is plunged into a warm (+37 C) warming solution containing low concentration of non-permeating cryoprotectant. This process happens within seconds. Oocytes or embryos are then moved through one or more wash drops containing reducing amounts of non-permeating cryoprotectants to ensure controlled dilution and removal of cryoprotectants and rehydration of cells. This process takes a few minutes.
Blastocysts, being more complex due to differentiation of embryonic cells into Inner Cell Mass and Trophectoderm and the presence of blastocoel cavity, may benefit from an additional step:
- 1) Artificial Shrinkage: Expanded blastocysts may undergo artificial shrinkage to reduce the risk of insufficient cryoprotectant penetration. This can be achieved by performing a breach either with a laser pulse or by using a micro manipulation tool to ‘nick’ the outer mass of cells, the trophectoderm. This will ensure that fluid within the blastocoel cavity is removed quickly, and the blastocyst shrinks rapidly. It is not always essential to manually shrink the blastocysts, and some embryologists prefer to use simpler methods to shrink the blastocyst using standard embryo handling pipettes and by pipetting blastocyst in and out of the pipette several times.
- 2) Equilibration, exposure to vitrification solutions and rapid cooling: Blastocysts are then vitrified following very similar processes used for cleavage stage embryos.
Benefits and Success Rates
Vitrification has shown higher survival rates and better clinical outcomes compared to the previous slow-freezing methods. Studies have also demonstrated that vitrified oocytes and embryos have similar survival and pregnancy rates to ‘fresh’ ones. This is particularly important for patients undergoing in vitro fertilization (IVF), where the quality and viability of oocytes and embryos play a critical role in the success of the procedure.
Future of Vitrification
The future of vitrification looks promising with ongoing advancements aimed at improving efficiency, embryo survival and outcomes are being developed. Key areas of focus include:
Standardisation:
Efforts are being made to standardise protocols to reduce variability and improve reproducibility across different laboratories.
Cryoprotectant Optimization:
Research is ongoing to develop new cryoprotectants that are less toxic and more effective.
Automation:
Automated systems like Genea Gavi® are being developed to streamline the vitrification process, reducing human error and improving consistency.
Fast Vitrification:
Speeding up the process of embryo equilibration during vitrification cooling and whole procedure during the warming process can make the technique easier for scientists to perform.


Reducing variability of Automatic Vitrification with Genea Gavi®
Genea Gavi® represents a significant advancement in the field of vitrification. This automated system offers several benefits:
Consistency and Precision:
Gavi® standardizes the vitrification process, ensuring consistent results by controlling critical parameters such as temperature, cryoprotectant concentration, and exposure time.
Reduced Learning Curve:
The system simplifies the vitrification process, making it accessible to embryologists with varying levels of experience.
Improved Outcomes:
Studies have shown that Gavi® can achieve high survival rates and improved clinical outcomes, making it a viable option for modern IVF laboratories.
Fast vitrification
Fast vitrification is a is a recent trend in embryo vitrification accelerating vitrification process while conveying overall benefits of vitrification. This method is gaining attention due to its potential to improve efficiencies, clinical outcomes and reduce the time required for cryopreservation processes.
In published studies these protocols have maintained similar or better survival and development rates compared to standard vitrification methods while significantly reducing execution times. The reduction in execution times was substantial, with time savings of up to 90% in laboratory settings obtained in some cases.
While fast vitrification shows promise, its clinical efficacy requires further validation. Published studies indicate high potential, but clinical trials or large sets of data may be needed to confirm the reliability and effectiveness of these protocols in large scale clinical applications. Additionally, the development of universal protocols that can be applied across different cell types remains a significant challenge.
In conclusion, fast vitrification offers a promising alternative to traditional cryopreservation methods by reducing execution times and minimising the negative effects of cryoprotectants.